Ibogaine, a naturally occurring psychoactive compound derived from the root bark of the African Tabernanthe iboga shrub, has garnered substantial attention in recent years for its potential therapeutic effects—particularly in the treatment of addiction and certain mood disorders. The growing interest has led to increasingly complex discussions around Ibogaine order, touching on everything from sourcing and legality to dosage and administration protocols. This article delves into what the term entails, why it’s important, how it’s navigated in medical and regulatory contexts, and what the future might hold.
The phrase Ibogaine order often appears in clinical, scientific, and policy discussions—generally referring to the precise specification of ibogaine in terms of dosage, formulation, administration method, and legal classification. Whether you’re a healthcare professional, researcher, or someone considering ibogaine therapy, understanding the nuances of this term is essential for both safety and efficacy. For an authoritative foundation on the compound, the Psychedelic Medicine Association provides a comprehensive resource outlining ibogaine’s pharmacology, history, uses, and regulatory context; you can explore further at Ibogaine order.
What Does Ibogaine Order Encompass?
Legal Classification and Regulatory Status
One major aspect of “ibogaine order” revolves around its legal classification across jurisdictions. Some countries regard ibogaine as a controlled substance, requiring special licenses or approvals for its medical use or research. Practitioners and institutions often need to navigate extensive bureaucratic frameworks—securing import permits, clinical trial authorizations, or compassionate-use exemptions.
On the other hand, in regions where regulations are more permissive, “ibogaine order” might simply refer to the procurement of pharmaceutical-grade material, conforming to safety and purity standards. Institutions must carefully document chain-of-custody, testing certificates, and dosing logs to comply with best practices and legal requirements.
Sourcing and Quality Assurance
Beyond regulation, “ibogaine order” also pertains to how the substance is sourced. There’s a vast difference between raw plant extracts, laboratory-synthesized batches, and standardized pharmaceutical preparations. Reliable providers supply certificates of analysis that indicate potency, purity, and absence of contaminants—a critical factor, given the compound’s potency and potential cardiovascular effects.
In clinical settings, “ibogaine order” may involve the issuance of standardized formulations—such as capsules or oral suspensions—facilitating consistent dosing. In more experimental contexts, dosage forms can include tinctures or powdered extracts, requiring additional calculation and quality control.
Clinical Dosing and Administration Protocols
One of the most crucial components of “ibogaine order” is the protocol specifying how it’s administered:
Screening and Pre‑Treatment Evaluation
Before any ibogaine order is enacted, patients should undergo comprehensive medical screening—cardiac function assessments (e.g., ECG), liver and kidney panels, psychiatric evaluation—to ensure they are suitable candidates. The order usually includes contraindications such as existing heart conditions, pregnancy, or interactions with other medications.
Dosing Ranges
Initial doses can range from 200 to 800 mg, depending on body weight, metabolic factors, and therapeutic goals. Some protocols distinguish between a “loading” dose (to initiate the psychedelic breakthrough) and subsequent “booster” doses to sustain therapeutic activity. The term “ibogaine order” captures this dosing regimen and its clinical rationale.
Monitoring and Support
Administering ibogaine carries risks, particularly to cardiovascular and neurological systems. A robust order will mandate continuous monitoring—heart rate, blood pressure, oxygen saturation, and mental state checks, typically in a facility equipped for medical emergencies.
Post‑Session Integration
A thorough ibogaine order doesn’t end with administration. Integration—the process of psychological support, therapy, and follow‑up—is vital. Orders may incorporate aftercare components such as counseling sessions, support groups, or outpatient medical checks to reinforce long‑term benefits and safety.
Scientific and Therapeutic Rationale
Mechanism of Action
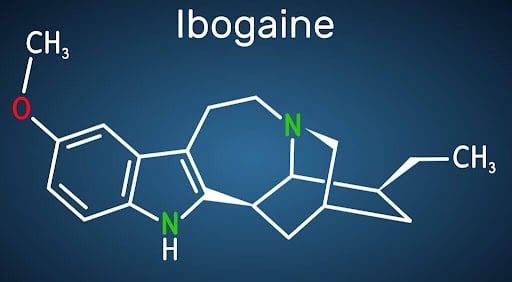
Ibogaine’s unique pharmacological profile sets it apart from many psychoactive substances. It interacts with multiple neurotransmitter systems—NMDA receptors, opioid receptors, serotonin transporters, and sigma-2 receptors—creating a “reset” effect in neural circuits implicated in addiction and mood dysregulation. Understanding this multi-target mechanism underpins the rationale for precise “ibogaine order” protocols.
Evidence Base and Clinical Research
Though rigorous, large-scale clinical trials remain limited, observational studies and anecdotal reports suggest significant outcomes—especially for opioid, stimulant, and alcohol dependence. Structured facilities adhering to well-defined ibogaine order protocols report high rates of early abstinence and subjective improvements in mood and self‑awareness.
Implementation Challenges and Ethical Considerations
Safety and Risk Management
With serious risks such as cardiac arrhythmias, hypotension, and neurotoxicity in overdose, any ibogaine order must be accompanied by medical supervision. The challenge lies in striking a balance: enabling potential benefits while minimizing adverse events through dose precision, patient selection, and emergency preparedness.
Equity and Access
Controlled or high-cost settings limit access to therapies like ibogaine. Even as some advocate for legal reform or compassionate-use frameworks to expand availability, the complexity of ibogaine order logistics—permits, clinical staff, facility requirements—often restricts access to affluent or medically complex populations.
Ethical Boundaries
Practitioners must navigate informed consent carefully—ensuring patients understand experimental status, potential side effects, and unknown long-term outcomes. Ibogaine orders should be transparent, standardized, and rooted in patient autonomy and safety.
The Future of Ibogaine Order in Therapeutic Contexts
Legislative shifts, evolving clinician attitudes, and increasing patient interest are driving momentum toward more structured integration of ibogaine in therapeutic settings. Standardizing ibogaine order frameworks—incorporating dosing guidelines, delivery systems, and monitoring protocols—can improve outcomes and bolster legitimacy. Training programs, research consortia, and cross‑jurisdictional collaborations may contribute to more consistent and safer implementation.
Conclusion
In summary, “Ibogaine order” encompasses much more than simply prescribing or obtaining the compound. It involves a nuanced process: understanding legal frameworks, ensuring quality, implementing precise dosing regimens, integrating monitoring and support, and upholding ethical standards. As interest in psychedelic-assisted therapy grows, refining and standardizing ibogaine orders will be critical for patient safety, therapeutic efficacy, and broader acceptance in medicine.
For those interested in exploring ibogaine further—from pharmacology to legal context—check out the authoritative source on ibogaine provided by the Psychedelic Medicine Association via the well‑documented Ibogaine order resource.
Finally, as professionals and learners engage with continuing education opportunities in this evolving field, resources relating to psychedelic medicine CE/CME offer structured avenues to deepen knowledge, uphold best practices, and stay current as the landscape of psychedelic therapy advances.